As I have supported several Health Condition Coding (HCC) engagements at KHC, I’ve been diving into the industry eyes wide open.
A recent Office of Inspector General (OIG) review of Medicare Advantage (MA) companies found that during 2016, the 162 MA organizations received $9.2 billion “from diagnoses that were reported only on chart reviews and HRAs, and on no other service records.”1 Of these 162 organizations, 20 received 54% ($5 billion) of the payments while accounting for only 31% of MA beneficiaries.
The Centers for Medicare and Medicaid Services (CMS) risk-adjusts capitated payments based on beneficiaries’ diagnosis codes. MA organizations report beneficiaries’ diagnosis codes based on service provided to the beneficiary to CMS’ MA encounter data system and the Risk Adjustment Processing System. There are two primary sources for MA organizations to identify diagnoses used for risk adjustment:
- Chart reviews are an MA organization’s review of a medical record to identify diagnosis codes that a provider did not submit or submitted in error.
- Health Risk Assessments (HRAs) occur when a health care professional collects information from the beneficiary about their health in order to diagnose a beneficiary and identify gaps in care.
The diagnosis codes are then translated into HCCs that are used for the basis of payments to MA organizations.
The OIG found that the HCCs based on chart reviews and HRAs were not always supported by services documented in the medical record:
HCCs generated by diagnoses reported only on chart reviews and HRAs included serious illnesses, such as diabetes and heart disease. However, there were no service records directly demonstrating that beneficiaries who had a chart review and/or HRA received treatment for these serious health diagnoses.
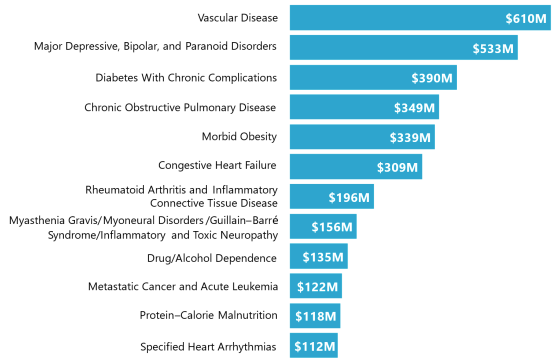
The OIG further identified that for the 20 companies, $3.4 billion (68%) of their total $5 billion in payments on HCCs based only on chart reviews and HRAS were on 12 of the 101 possible HCCs, as identified in the chart from their report as displayed below.
The OIG recommended that CMS should provide oversight to these 20 MA organizations and perform “periodic monitoring to identify MA companies that had a disproportionate share of risk-adjusted payments from chart reviews and HRAs.”
Providers and MA organizations should pay close attention to the findings and establish procedures to ensure that risk-adjusted diagnosis codes are supported by services documented in the encounter notes.
At KHC, we advise our clients to establish and HCC coding workflow that integrates the doctor and an HCC coder, in order to ensure that all diagnoses are supported and that HCCs are appropriately captured. This workflow is supported by data mining and analytics to identify high risk areas and monitor the success of the HCC program. We recommend our clients consider the following:
- Analyzing data available from the Medicare Advantage (MA) plans, such as Open HCC Lists and MA websites, to calculate and monitor HCC recapture rates. This data can also be used to identify and schedule patients with open HCCs.
- Monitoring volumes of frequently miscoded diagnosis codes/HCCs (e.g., heart attack or active stroke within office), especially those on the OIG’s list above.
- Monitor diagnosis codes submitted on encounters by providers that cannot assign risk adjusted diagnosis codes.
- Monitor the volume of diagnosis codes that are unspecified, as the medical record may support a higher level of specificity.
- Use patient measurements taken during an office visit and recorded in the medical record, such as body mass index (BMI), to identify inappropriate diagnosis codes (e.g., cannot be morbidly obese if BMI is low).
Resources
- Office of Inspector General report, “Some Medicare Advantage Companies Leveraged Chart Reviews and Health Risk Assessments To Disproportionately Drive Payments”: https://oig.hhs.gov/oei/reports/OEI-03-17-00474.pdf
Data problem? Analytics? Regulations? Data privacy? Humanity? Coffee and talk? You can reach me at jleventhal@kohlerhc.com or 312.933.2752.
Josh Leventhal is an expert in healthcare data and analytics and is Managing Director with Kohler HealthCare. He has over 15 years of hands-on experience in healthcare data and analytics solving problems for providers, payers, and life science organizations. Josh started his career in management consulting analyzing data for the largest joint defense litigations in the country before applying his skills and expertise at local startups to assist the Medicaid a managed care organization and medical research industries. His experiences as a consultant, product manager and developer allow him to work effectively with both business and technology stakeholders.



